Table of Contents
ToggleWhat are Arteries?
Arteries are the blood vessels that carry oxygen-rich blood from the heart to all parts of the body. When arteries become blocked or narrow, a condition called peripheral arterial disease or peripheral artery disease (PAD) occurs. The symptoms may give people clues about its presence—such as leg pain when walking or slow-healing wounds on the feet—but don’t appear until the disease is more advanced.
What is the Difference between Peripheral and Systemic Arteries?
Peripheral arteries are the blood vessels that branch out from the aorta and carry blood towards the smaller arteries and arterioles, which supply oxygenated blood to different parts of our body. Systemic arteries (also known as distributing arteries) generally refer to the larger branches of the aorta and they carry oxygenated blood throughout your body.
What is Peripheral Artery Disease?
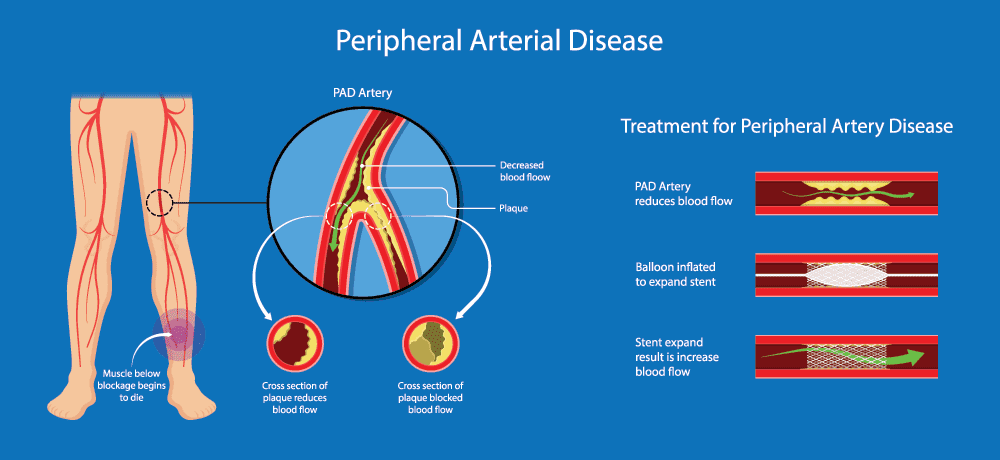
Peripheral arterial disease is a condition where there is a blockage in the blood vessels that carry blood from the heart to the feet. This can cause pain in the calves when walking or exercising, cramping in the calf muscles after exercise, and changes in your skin color (pale or blue). The risk of cardiovascular disease increases with age for everyone; however, PAD typically affects older adults who are over 50 years old. It is very common for people to have PAD without any symptoms; therefore, it may go untreated. For this reason, it is important for individuals over 50 years old to know their risks for developing PAD and what they can do to prevent serious health problems like stroke and heart attacks.
How Many People Have Peripheral Artery Disease?
2% of people over 70 years age have PAD. PAD is a major risk factor for heart attacks and strokes, which means that PAD raises the risk of these events. It is estimated to affect at least 8 million Americans1 and can be found in people as young as 30 years old. According to the Centers for Disease Control and Prevention (CDC), approximately 500,000 people in the United States have a heart attack each year.
Although PAD is a serious condition that can affect daily life—and even shorten it—it can be treated and managed well with proper education about how to manage symptoms and monitor the disease.
What Causes Peripheral Arterial Disease?
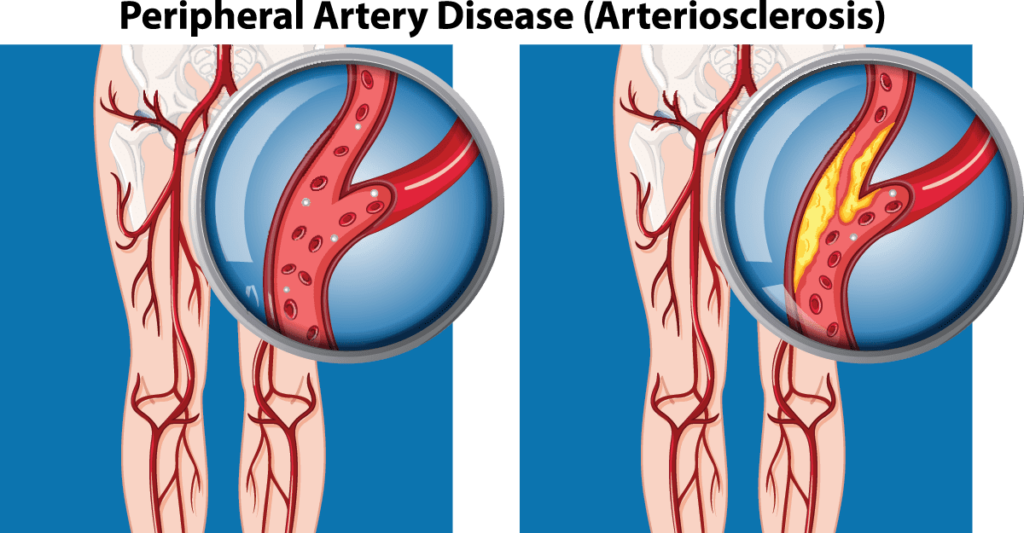
PAD occurs when arteries become narrowed or blocked by fatty deposits called plaque, reducing blood flow. The condition may develop due to the build-up of plaque over time, a disease called atherosclerosis . Atherosclerosis can affect any artery in the body and is often associated with other chronic diseases such as:
- Type 2 diabetes
- High blood pressure
- High cholesterol
- Overweight or obesity (body mass index greater than 30)
- Increasing age
- Family history of peripheral arterial disease, heart disease or stroke
In about one-third of people with PAD, the cause is unknown. Men are more likely to develop PAD than women. Some risk factors for PAD may be out of a person’s control but others—such as smoking and unhealthy diet—can be controlled through lifestyle changes.
Less common causes of peripheral arterial disease include other diseases such as vasculitis, birth defects, injury to the blood vessels, certain medications, and other factors.
What are Risk Factors for Developing Peripheral Artery Disease?
Peripheral artery disease can run in families, so genetic factors may play a role. But the main risk factors are more controllable, including:
- Smoking – Smokers with smoking-free lungs had a shorter life expectancy and more frequent progression toward limb ischemia and amputation compared to nonsmokers in one study.
- High blood pressure – is a major risk factor for developing cardiovascular disease and can damage the arteries.
- Prior heart attack or stroke – increases the risk of future heart attacks and strokes, so it’s important to take preventive measures such as controlling high blood pressure and cholesterol levels.
- Diabetes – diabetes damages blood vessels, increasing the risk of PAD.
- Being overweight – is closely linked to diabetes, which increases the risk of heart disease and PAD.
- Physical inactivity – those who are inactive or bedridden have an increased risk of developing PAD.
- Age – As people age they are more likely to develop hardening of the arteries
What the Symptoms of Peripheral Artery Disease?
Often, there are no signs or symptoms in early stages of PAD. When they do occur, the most common complaint is leg pain when walking (called claudication). It happens because narrowed arteries reduce blood flow to muscles in the legs and lower extremities. The walls of the affected arteries may also become thick and stiff, especially in the lower leg. Fatty plaque buildup on artery walls cause the blocked arteries to deliver less blood flow to leg muscles and PAD symptoms result.
As the disease progresses and blood flow becomes more compromised, symptoms may include:
- Numbness or tingling of the foot, ankle or leg
- Sores on your feet that heal slowly
- Leg pain at rest
- A cool sensation
- Footdrop—the inability to raise up your forefoot because your calf muscle has tightened due to nerve damage
- Weakness in the legs (can lead to falls)
- Hair loss or slow hair growth
- Shiny skin
- Slow growth of your toenails
These are warning signs to seek help and an early diagnosis. The symptoms of PAD typically appear on one side of your body (unilateral involvement). However, symptoms can also occur in both lower extremities at the same time (bilateral involvement).
Does Diabetes Cause Peripheral Artery Disease?
Yes, in some cases. In a person who has diabetes, excess sugar in the blood damages blood vessels and reduces blood flow. This change in circulation can lead to atherosclerosis. Atherosclerosis is the narrowing of an artery that results from the buildup of fatty deposits on the inner walls of arteries (plaque). This process can cause symptoms of peripheral arterial disease.
Does Smoking Cause Peripheral Artery Disease? And What is Buerger’s Disease?
Yes. Smoking damages the lining of blood vessels, which makes them more fragile and likely to rupture. This increases the risk of peripheral arterial disease in people who smoke or have stopped smoking recently. Cigarette smoking may also contribute to Buerger’s disease, a condition that causes narrowing of blood vessels in the arms and legs similar to PAD.
What are Risk Factors for Buerger’s Disease?
Buerger’s disease is rare, but it impacts men more than women and tends to develop at a younger age . Other risk factors for Buerger’s disease include:
- Smoking – more than 80 percent of people who develop Buerger’s disease are smokers
- Tobacco use at a young age – if you started smoking before age 21, it may increase your risk of developing Buerger’s disease
- Black race – people of African descent have higher rates of Buerger’s disease than Caucasians
- Exposure to certain toxins such as carbon disulfide, used in the rubber industry
- Personal or family history of Buerger’s disease
- Infection with certain viruses – Epstein-Barr virus and hepatitis C Drug use
How is Peripheral Arterial Disease Diagnosed?
If you have symptoms such as leg pain when walking, see your doctor. He or she may ask about your symptoms and medical history and perform a physical exam to look for signs of PAD.The doctor will ask about:
- The location and severity of the pain
- How long it lasts
- What makes it worse (walking up stairs, at night while in bed).
The doctor also will want to know:
- Whether there are any other symptoms such as numbness or tingling in the toes or lower legs
- How well oxygen is reaching the rest of the body
- Whether you have had an injury to that area
- Your age and family history
- If any past surgeries were performed on that limb
An assessment risk factors including smoking, high blood pressure, diabetes and family history. Blood tests will likely be done to assess the function of the heart and circulation system. The doctor may suggest other tests such as:
- A Doppler ultrasound—a test that uses high-frequency sound waves to determine how much resistance there is in a blood vessel (resistance increases when blood flow is blocked). An ultrasound can also show narrowing or blockage in an artery.
- An angiogram —uses X-ray techniques to look at arteries inside the body to see if they are narrowed or blocked
- A CT scan—an imaging technique that uses X-rays and computers to create detailed images of your internal organs. A computer performs rapid, multidetector scans during which thin slices of the body are scanned and displayed to create cross-sectional views of internal structures such as bones, blood vessels and organs.
- A magnetic resonance angiogram (MRA) —uses a combination of large magnets, radio frequencies and a computer to produce detailed images of your arteries and veins without using X-rays
- A CT angiogram —a type of CT scan that uses contrast dye to provide greater detail than an MRA
- A Doppler ultrasound—a test that uses high-frequency sound waves to determine how much resistance there is in a blood vessel (resistance increases when blood flow is blocked). An ultrasound can also show narrowing or blockage in an artery.

Can Peripheral Artery Disease Be Prevented?
Yes. Try and maintain a healthy lifestyle including:
- Avoid smoking
- Quit smoking
- Maintain a healthy weight
- Exercise regularly
- Eat food low in saturated fat
- If you have diabetes control your blood sugar level
- If you have hypertension control your blood pressure
- If you have high cholesterol talk to your doctor about ways to decrease it
What are the Treatment Options for Peripheral Artery Disease?
The goal of treatment is to improve blood flow in your legs so you can walk farther or more comfortably without pain. The doctor will determine which treatment may be right for you based on factors including:
- How severe your symptoms are
- Whether the condition has been diagnosed recently
- Your age, general health and other medical problems
Treatment may include:
Walking regularly—walking several times each day helps keep blood circulating through your body efficiently. “Showering” cold water over your legs for five minutes after walking also helps keep blood circulating.
One or more of the following:
Medications—aspirin, clopidogrel (Plavix) and pentoxifylline (Trental), can help improve blood flow in your legs. These may be taken long-term or short-term depending on your condition. You doctor will decide which medicine is right for you and how long to take it. If you have diabetes, these medications may affect how much insulin you need so tell your doctor if you have diabetes before taking aspirin, clopidogrel or pentoxifylline.
Nonsteroidal anti-inflammatory drugs such as ibuprofen (Advil, Motrin) can help relieve pain associated with walking.
Topical nitroglycerin ointment, sprays or patches that you apply to your skin—when combined with other therapies, these may improve blood flow in your legs and reduce the symptoms of claudication.
What Nonsurgical Options Other for Peripheral Artery Disease?
Imaging and interventional specialists not only have in office diagnostic technologies but can offer modern, cutting-edge treatments to increase circulation in the legs and feet.
Below are some therapies offered by our vascular specialists:
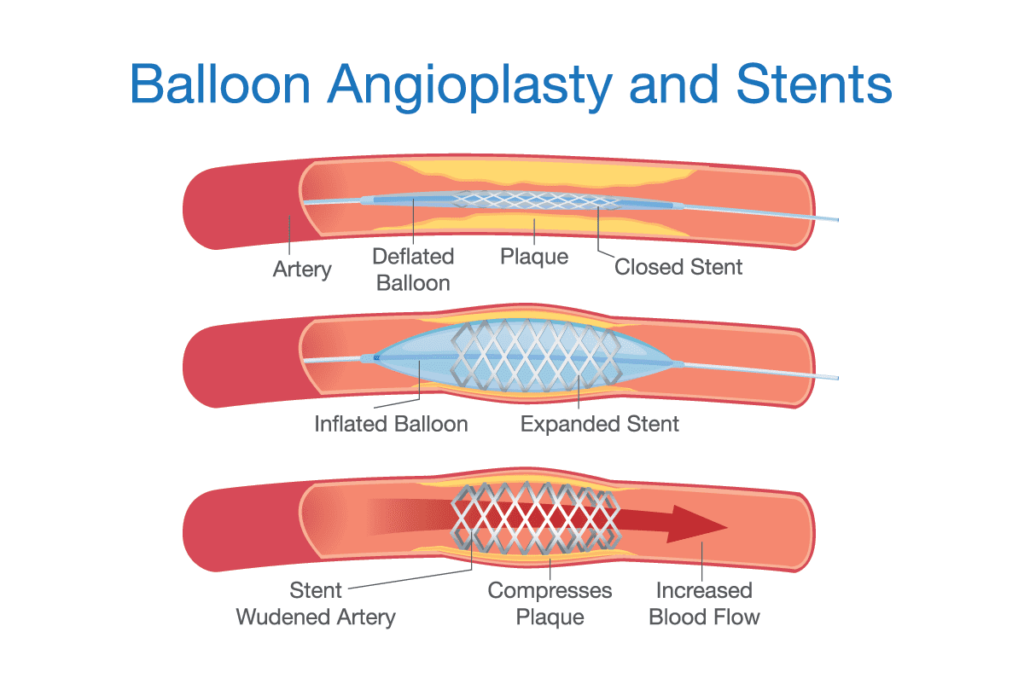
Balloon angioplasty – a non-surgical treatment where a catheter-mounted balloon is placed inside your arterial system and inflated to treat arterial narrowing.
Stenting – a procedure in which a wire mesh tube called a stent is inserted inside an artery to keep it open and increase blood flow through the vessel. The doctor will also perform an angioplasty at the same time to make sure your leg does not go back to its weak state.
Atherectomy – a non-surgical procedure in which a catheter-mounted device is inserted into your artery to remove plaque or scar tissue that causes the narrowing of the vessel.
What are Advanced Symptoms of Peripheral Artery Disease?
Advanced symptoms of severe PAD may include:
- An ankle, foot or leg wound that fails to heal
- Paralysis and weakness in your legs and/or feet due to poor blood flow
- Poor muscle tone and loss of feeling in your legs and feet
- Changes in the color and temperature of your lower leg(s), such as a bluish-white color or cold, numb skin
- Severe pain that keeps you from walking even short distances. You may notice decreased sweating or changes in the appearance of your feet such as darkening of the skin on one side compared to the other. If you have diabetes, this can affect how much insulin you need so tell your doctor if you have diabetes before seeing a vascular
What is Claudication?
Claudication is a symptom of peripheral arterial disease. It refers to leg pain that occurs during exercise, such as walking or climbing stairs, and subsides when you stop exercising. When claudication is caused by PAD, it’s due to poor circulation in the legs and feet. This makes it harder for blood to reach the muscles needed for movement. As a result, your muscles don’t get enough oxygen-rich blood. This causes pain. If you have claudication, the pain usually lasts for more than a few minutes and goes away quickly when you stop walking.
What are Arterial Nonhealing Ulcers?
An ischemic ulcer, also called an arterial ulcer, is a serious complication of peripheral artery disease. It is caused by lack of blood supply to the tissues in your leg. Without treatment, an arterial ulcer can lead to gangrene and even amputation. An arterial nonhealing ulcer is a wound that won’t heal due to poor circulation in the legs and feet. People with peripheral arterial disease who have tissue death from poor blood flow are most at risk for this kind of wound.
When Should I Seek Medical Help for My Leg Ulcers?
If you notice any signs of infection around an ulcer — such as swelling, warmth, redness or fluid draining from the wound — contact your doctor immediately. You might also contact your doctor if you notice new ulcers or if existing ulcers appear to be getting worse.
What Is Critical Limb ischemia?
Critical limb ischemia (CLI) occurs when a lack of blood flow in your leg(s) cuts off all oxygen to the tissue below your knee or mid-calf. If not treated, you may require an amputation. CLIs most often affects people with diabetes, smokers and those who have poorly controlled blood pressure.
What is Gangrene?
Gangrene is the death and decay of tissue in an arm or leg due to a severe lack of blood flow and oxygen. Gangrene often begins in one part of your body, such as your toes. If not treated quickly, gangrene can spread throughout your entire limb and it may become necessary to amputate.
What are Surgical Options for Peripheral Artery Disease?
If nonsurgical therapies fail to improve blood flow in your legs and feet, you may require a surgical amputation. This is often the only way to save your life.
Amputation is performed when other methods of revascularizing blood vessels to restore circulation are unsuccessful, or when other options may result in major complications for you. Generally speaking, gangrene (tissue death) must be present before an amputation can be done because the wound may heal if given time and proper care. Surgery usually involves removal of the limb below the knee or mid-calf. An arterial nonhealing ulcer that develops into gangrene is a common reason why someone would require an amputation.
Management of Peripheral Artery Disease
Peripheral artery disease can be managed either nonsurgically, or if critical limb ischemia and gangrene cannot be treated, surgically with amputation. Nonsurgical management includes medical management and endovascular treatment.
Nonsurgical Management:
Medications — such as platelet inhibitors, vasodilators and anticoagulants — are used to treat peripheral arterial disease. They help prevent further blockage of blood flow in your legs and feet. By lowering your cholesterol, these medications may also reduce future risk for heart attack and stroke.
Endovascular therapy — a noninvasive procedure that uses specialized catheters to insert a stent into the affected artery to open up the blood vessel. This is done at an outpatient center under local anesthesia with minimal downtime.
Surgical Management:
If you’re diagnosed with severe peripheral arterial disease, amputation may be required. Amputation is performed when other methods of revascularizing blood vessels to restore circulation are unsuccessful, or when other options may result in major complications for you. Generally speaking, gangrene (tissue death) must be present before an amputation can be done because the wound may heal if given time and proper care. Surgery usually involves removal of the limb below the knee or mid-calf. An arterial nonhealing ulcer that develops into gangrene is a common reason why someone would require an amputation.
How Do Imaging and Interventional Specialists Find Out Whether You Have Peripheral Arterial Disease?
The Imaging & Interventional Specialist team has in office diagnostic technologies to help identify whether you have peripheral arterial disease and how severe it is. Besides our careful history and physical exam, the team at Imaging & Interventional Specialists may obtain ultrasound studies, blood pressure measurements (ankle-brachial index), tissue oxygenation levels, angiography or other advanced imaging (for example Magnetic Resonance Imaging) to aid with accurate diagnoses and help develop your treatment plan, if needed.
What Advanced “Pinhole” Procedures Do Imaging and Interventional Specialists Offer for Peripheral Artery Disease?
For peripheral artery disease (PAD) Imaging & Interventional Specialists will determine if non-surgical vascular interventional radiology (VIR) procedures can address your situation or whether lifestyle changes, treatment of pre-existing conditions, or surgery is a better option. Lifestyle changes include exercise and quitting smoking. Aggressive treatment of diabetes, high blood pressure and high cholesterol is important. Medicines that improve blood flow and relax the blood vessels may also be of benefit.
For peripherial artery disease Imaging & Interventional Specialist MDs may obtain ultrasound studies, blood pressure measurements (ankle-brachial index), tissue oxygenation levels, angiography or other advanced imaging (for example Magnetic Resonance Imaging) to aid with accurate diagnoses and help develop your treatment plan, as needed.
Angiography (taking pictures of your arteries to diagnose where there are problems)
Angioplasty (introducing a small balloon to open up areas that are closed due to plaque)
Stent placement (placing a cylindrical brace to hold your artery open)
Atherectomy (introducing a tiny instrument that will crear some of the plaque on the inside of your disease artery)
Imaging & Interventional Specialists “Pinhole” Procedures: Fast Recovery, Less Risk, Less Pain, Comfortable Setting
Our experienced board-certified specialists successfully perform “pinhole” procedures every day offering this region leading, state-of-the-art solutions to peripheral artery disease.. Our non-surgical image guided procedures are cutting edge technology without the cutting, without the scalpel. You leave with a Band-Aid!
- Procedures are usually done in a comfortable outpatient setting with familiar friendly staff
- Pinhole procedures offer fast recovery, less risk, and less pain
Why Imaging & Interventional Specialists?
Imaging & Interventional Specialists are leaders in interventional radiology and experts in the non-surgical procedures that will cure or minimize your peripheral vascular disease
Using state-of-the-art equipment, our experienced board-certified specialists are focused on your best outcome.
Early detection is vital. It is important to determine whether you have peripheral arterial disease since this can progress to gangrene due to critical limb ischemia. At Imaging & Interventional Specialists board certified physicians offer in-house testing to determine the cause and develop an individualized treatment program for your peripheral arterial disease.


