Table of Contents
ToggleWhat is the Difference between a Vein and an Artery?
A vein is a blood vessel that carries blood toward the heart. An artery is a blood vessel that carries blood away from the heart.
What are Varicose Veins?
Varicose veins are enlarged twisted veins. They often look rope-like or “wormy.” Varicose veins can occur anywhere in the body but they most commonly occur in the legs. Varicose veins affect people by being unsightly and painful. The skin overlying varicose veins may also be itchy and burning. With time, this skin may become thickened and darkened (hyperpigmented). Although varicose veins can develop at any age, they more frequently develop after pregnancy, prolonged sitting or standing, obesity, injury to the leg, or prolonged inactivity. If they are not treated, varicose veins may eventually lead to more serious problems in the affected leg.
How Does Blood Flow Cause Varicose Veins?

Varicose veins are enlarged twisted veins. They often look rope-like or “wormy.” Varicose veins can occur anywhere in the body but they most commonly occur in the legs. Varicose veins affect people by being unsightly and painful. The skin overlying varicose veins may also be itchy and burning. With time, this skin may become thickened and darkened (hyperpigmented). Although varicose veins can develop at any age, they more frequently develop after pregnancy, prolonged sitting or standing, obesity, injury to the leg, or prolonged inactivity. If they are not treated, varicose veins may eventually lead to more serious problems in the affected leg.
How Do You Develop Varicose Veins?
The main cause of enlarged veins in the lower extremities is prolonged standing in otherwise healthy persons. These persons likely have a genetic predisposition for developing weak vein walls that fail to support the high pressure within the vein system when they stand for long periods (such as during pregnancy). Varicose veins can also develop in people with an inherited weakness of valves in the small veins; these people are also more prone to blood clots. The same risk factors listed above can cause chronic venous insufficiency (CVI), which is one type of chronic venous disease (CVD). Other types of CVD include superficial venous reflux and deep venous reflux disease.
People with CVI typically have aching, throbbing, or cramping pain in their legs that gets worse as they walk or stand for an extended period.
Leg swelling is more common than leg pain and is usually more severe than other types of chronic venous insufficiency. Leg swelling occurs because the valves inside the veins do not open properly and allow blood to pool in certain areas of your legs. The more time you spend standing or walking, the harder your muscles work to push the blood back up to your heart (a process called “venous return”). The effort required by these leg muscles can cause swelling in your feet, ankles, or legs.
What Happens with Faulty Valves?
Varicose veins are the result of faulty valves in the veins that reduce blood flow back to the heart, allowing it to pool in these vessels instead. The valves become weak and stretch out over time. As this process continues, varices begin to form and become even more obvious. This is normal aging of valves within veins; however, in some cases, damage to valves can be due to other factors. Once they develop, varicosities do not go away on their own. However, if given proper treatment by a vein specialist (vascular surgeon) most people with leg varicosities can enjoy relief from symptoms and improved quality of life.
Are Varicose Veins Dangerous?
Most people with varicose veins do not have any health problems related to them. However, in some cases, varicose veins can lead to more serious problems such as:
- Chronic venous insufficiency (CVI): This is a condition in which the valves inside the veins do not open properly and allow blood to pool in certain areas of your legs. The more time you spend standing or walking, the harder your muscles work to push the blood back up to your heart (a process called “venous return”). The effort required by these leg muscles can cause swelling in your feet, ankles, or legs.
- Deep vein thrombosis (DVT): This is a serious condition in which a blood clot forms in one of the deep veins in your body. DVT most often occurs in the lower leg, but it can also occur in other parts of the body. If a blood clot breaks free from its original location and travels to the lungs, it can cause a pulmonary embolism (PE),
Who is Likely to Get Varicose Veins?
People are likely to develop varicosities if they have a family history of them or if they:
- Are pregnant or just had a baby. The weight and pressure of the uterus on the inferior vena cava increases pressure in leg veins and may cause them to enlarge and become varicosities.
- Have an inherited weakness in vein walls and valves. This makes the vein more likely to fail under high pressures when standing or sitting for long periods. Sitting for too long, such as working at a desk, watching TV, or traveling by car can increase pressure within leg veins and worsen symptoms. Some people with this type of CVD don’t even get varicose veins until they sit for prolonged periods;
What are the Risk Factors for Developing Varicose Veins?
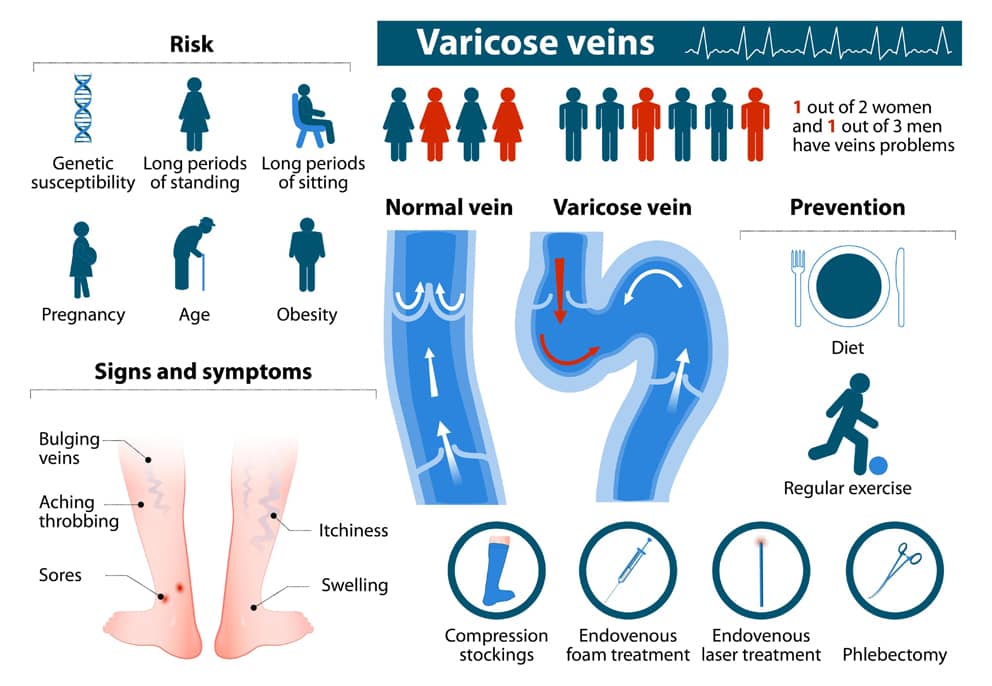
Risk factors that can lead to varicose veins or chronic venous disease include:
- family history of varicose veins
- standing for long periods
- sitting with legs crossed or putting pressure on the veins
- obesity
- being a woman – in part due to pregnancy
- age
Deep vein thrombosis (DVT) is also a serious concern with persons suffering from varices or other forms of chronic venous insufficiency since it can lead to pulmonary embolism, a potentially fatal condition.
How are varicose veins diagnosed?
What Do Varicose Veins Look Like?
The appearance of varicose veins is usually characterized by a twisted and rope-like protrusion, most commonly found in the legs. However, they can also be found in other parts of the body such as the arm, penis, and vulva. The color of this vein may vary but is usually blue or purple. Varicose veins grow larger over time and become less resilient to blood flow. If blockages develop this causes extreme pain because pressure has been built up behind them. Some people believe that several factors contribute to their enlargement although it is believed that genetics plays a major role in who develops them; they tend to run in families due to an inherited faulty gene for example collagen.
What are the Stages of Varicose Vein Disease?
There are five stages of varicose vein disease each progressively worse:
1. Reticular Veins (Spider Veins)
Reticular veins are the most common type of varicose vein and usually appear on the legs. Reticular veins develop as a small bundle of closely packed, short red lines that often look like a spider web or tree branch pattern. They can also resemble corduroy material. This is probably due to their close spacing and crisscrossed arrangement.
Reticular veins are not dangerous in themselves but they may be an early sign of more serious vein disease developing below them.
2. Varicose Veins
Varicose veins are enlarged, twisted veins that have lost elasticity due to damage from chronic pressure (standing, etc.). In addition, valves inside these particular veins have been weakened which leads to backup of blood flow and a greater chance of clot formation.
3. Swelling of Legs and Ankles
The third stage of varicose vein diease involves swelling the the legs and ankles. This is caused by a buildup of blood in the lower part of your body. The swelling may extend all the way to your toes.The swelling and pain gets worse with standing or sitting for long periods of time. If you notice that your shoes are getting tight, this could be a sign of varicose veins.
4. Skin Discoloration (Lipodermatosclerosis)
The fourth stage of varicose veins is skin changes to the legs and ankles. This happens because the blood pools in the lower part of your body, causing blood clots (thrombophlebitis) or redness (erythema). The skin color may become darker than usual due to increased pressure on nearby tissue. The skin may also become thick, shiny, and itchy with time when the nerve endings are damaged by changes in blood pressure.
Skin discoloration is usually more noticeable on the front of your legs. Sometimes doctors call this stage lipodermatosclerosis because of how it looks – like someone has used lipstick or lip balm to outline the affected area of skin. Discolored skin is often more painful than before. It can get more severely swollen with time if too much blood pools in one place for a long period of time.
5. Ulcers and Open Sores
Severe varicose veins can lead to ulceration and weeping can occur. Leg ulcers are open sores that do not heal easily. Skin ulcers are sores that develop on top of red or darkened skin due to excess pressure from pooled blood for an extended amount of time. Ulcers often occur up near the skin’s surface, but if they become deep enough they can reach down to the muscle and bone where you feel them as a dull aching pain.
What are Venous Ulcers?
To properly treat ulcers, we must first define what they are and how they occur. Ulcers are open sores that do not heal easily.
There are two types of ulcerations: venous and arterial ulcers. Venous ulcers form because the valves in your veins can no longer prevent backflow. Blood pools in the lower part of your body and damages nearby tissue. Arterial ulcers (also called ischemic ulcers) develop when the arteries cannot provide enough oxygen to a particular area, usually near the toes and feet; sometimes referred to as diabetic foot syndrome. Unfortunately, this type of ulcer is often the most serious.
Treatment is different for each type of ulceration. Arterial ulcers are treated with medications to open up blood vessels so more oxygen can reach the damaged tissues. Venous ulcers are treated by improving swelling, nourishing the skin, and strengthening the surrounding veins with sclerotherapy or other treatments.
How Do You Get Varicose Veins?
Varicose veins form when your leg veins become enlarged, twisted, or weakened from repeated pooling of blood in your legs because of gravity, pregnancy, trauma , hormonal changes, etc. These valves are supposed to keep blood flowing toward your heart. But if they become weak or diseased these damaged valves fail. Blood will move in whichever direction gravity pulls it which results in problem veins usually in the legs and feet.
What are the Common Symptoms of Varicose Veins?
Common symptoms include:
- Swelling or discomfort in the lower legs
- Stitches, aching numbness, tenderness, tingling, throbbing, itchiness in your legs
- General leg fatigue and weakness
- Visible varicose veins
How Do You Diagnose Varicose Veins?
A thorough medical history and physical exam are usually enough to make an accurate diagnosis; however diagnostic tools such as duplex ultrasound can confirm venous insufficiency. Other tests may be necessary if complications are suspected. A duplex will allow your physician to see both obstruction of blood flow (stenosis) and reflux back up toward the heart (regurgitation). These tests must be performed by a well-trained and experienced vascular radiologist.
What are the Risks Associated with Varicose Veins?
The risks associated with varicose veins can vary depending on the underlying cause. Some of the most common risks include:
- Venous ulcers. These are open sores that can develop if blood pools in the lower leg for an extended period. Venous ulcers can be difficult to treat and often require surgery.
- Bleeding. Vein disease can make you more likely to bleed from injuries, even small ones.
- DVT (deep vein thrombosis). This is a dangerous condition that can occur when a blood clot occurs in deeper veins.
What Treatments are Available for Varicose Veins?
Treatment for varicose veins can involve:
- lifestyle changes
- surgical interventional
- non surgical interventions
What are Lifestyle Changes that can Help Varicose Veins? How can You Prevent Varicose Veins?
Some basic measures that can be taken to prevent the development of varicose veins include:
- Exercise regularly. Walking is a good exercise for your legs because it helps improve blood circulation.
- Elevate your legs when resting. This will help reduce the pooling of blood in your lower extremities.
- Avoid standing or sitting for long periods. Take breaks to walk around every hour or so.
- Wear compression stockings. Compression stockings put pressure on the surface of your skin and help keep blood from flowing backward. They come in different levels of compression, so be sure to get a pair that’s right for you.
- Lose weight if you are overweight or obese. Maintain a healthy weight.
- Don’t cross your legs when sitting
- Avoid wearing tight clothing around your waist or legs
What are Surgical Interventions for Varicose Veins?
Vascular surgery interventions are rarely used in modern vascular practice but have included:
- vein stripping
- vein ligation
Vein stripping involves the surgical removal of the veins that are causing problems. Stripping often leads to the development of new varicose veins as well as smaller varicose veins so it should never be done again.
Vein ligation is the tying off of veins to prevent blood from flowing through them. Neither of these procedures is used very often anymore due to their risks and poor results.
What are Non-surgical Interventions for Varicose Veins?
Modern non-surgical interventions include:
- compression therapy
- sclerotherapy
- radiofrequency ablation therapy
- endovenous laser ablation
- Compression therapy – is the most common and least invasive medical treatment for varicose veins. It involves the use of special stockings or wraps that put pressure on the surface of your skin and help keep blood from flowing backward. This often fails to resolve the underlying problems. Compression stockings are available from medical supply stores.
- Sclerotherapy – is when the doctor injects a special solution into the veins. This solution causes the vein to collapse and be reabsorbed by your body.
- Microsclerotherapy – is an outpatient procedure that treats only the smaller, superficial spider veins near the surface of your skin using special injections. It does not involve incisions or stitches and takes less than half an hour to complete if several injections are needed for one leg. You can resume normal activities immediately after treatment but it may take months for full results so you must follow up regularly.
- Radiofrequency ablation -of varicose veins involves the use of a special probe that emits radiofrequency energy. This energy is used to heat and destroy the vein.
- Endovenous laser ablation – of varicose veins involves the use of a special laser fiber that’s inserted into the vein. The energy from the laser is used to heat and destroy the vein. Laser treatments are effective even with larger veins.
Both of these procedures are non-surgical and can be done in an outpatient setting with little downtime. These offer the best results even for larger varicose veins.
What are the Best, Most Up-To-Date Methods to Treat Varicose Veins?
Generally, endovenous radiofrequency ablation and laser treatment are considered the best procedures. And they are newer and more effective than sclerotherapy, vein stripping, and vein ligation.
What are the Advantages of Imaging & Interventional Specialists’ “Pinhole” Procedures

Our seasoned, board-certified specialists successfully perform “pinhole”, non-surgical procedures every day. We offer this region world class, state-of-the-art solutions for varicose veins. Our non-surgical image-guided procedures are cutting-edge technology without the cutting, without the scalpel. You leave with a Band-Aid!
- Procedures are usually done in a comfortable outpatient setting with familiar friendly staff.
- Pinhole procedures offer fast recovery, less risk, and less pain
Why Imaging & Interventional Specialists
Imaging & Interventional Specialists are leaders in interventional radiology and vascular medicine and experts in the non-surgical procedures that will address your varicose veins and relieve symptoms.
Using state-of-the-art equipment, our experienced board-certified specialists are focused on your best outcome.
At IMAGING & INTERVENTIONAL SPECIALISTS board-certified physicians offer in-house testing to evaluate you and to determine whether you have varicose veins. We develop an individualized treatment program for your varicose veins for your best outcome.

